Be warned, this post is a long one! The last couple of weeks have been quite stressful, as we have started the next phase of Chester’s chemotherapy. But the stress has mainly come from being admitted into the hospital, having to stay longer than expected, and the unorganisation and chaos from being in there.
If you read our last post, I spoke about the clinical trial and that Chester has been put onto the COGAALL1631 American experimental Arm B. So after both his inductions and bone marrow results, he started the first part of his frontline chemo treatment.

This phase is called HD MTX Interim Maintenance (IM) SR Arm and lasts 9 weeks, but longer if his counts are too low at certain points.
So the first round of chemo involved Chester going into his treatment center hospital for the first cycle. Day 1 started on Monday 19th August and he received his dose of Vincristine on the first day, which will be given every other week.
The next chemo he had to have was the HD MTX (High Dose Methotrexate). He has had IT Methotrexate several times which is given through his lumbar puncture and goes directly to his spinal fluid and brain. The High Dose Methotrexate is basically to go around the rest of his body.

Methotrexate is a medicine mainly used to treat some kinds of cancer, autoimmune diseases, and ectopic pregnancies. It works by blocking an enzyme called dihydrofolate reductase, which is needed for making DNA and helping cells grow. By doing this, methotrexate can slow down the growth of fast-dividing cells, like cancer cells and those involved in the immune system.
Because it is such a high dose and it’s quite a toxic medicine, Chester needed to be admitted for a couple of days to keep an eye on him and monitor the levels in his blood and urine. The idea is to get the medicine in, let it do its job, and then flush it out of his body as quickly as possible to avoid any damage and reduce side effects.
To begin with, Chester had to go on IV fluids through his central line. He needed to be fully hydrated and also they had to keep testing his urine as it has to be a certain PH level. It needs to be at 7 on the scale, which is a neutral number.

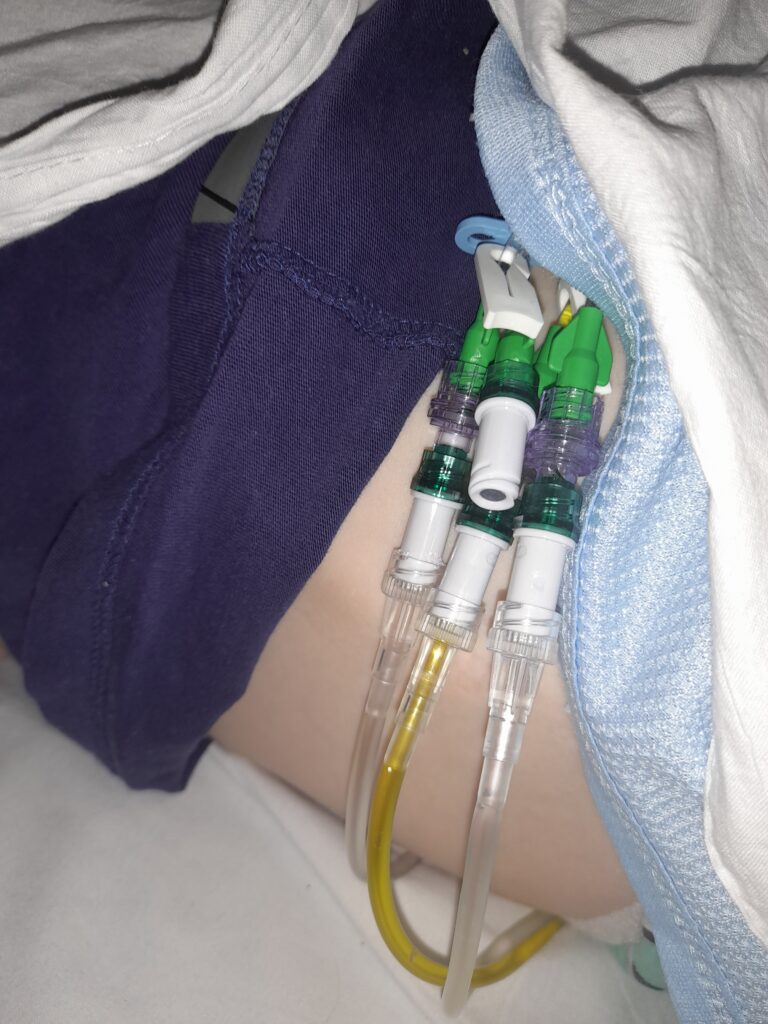
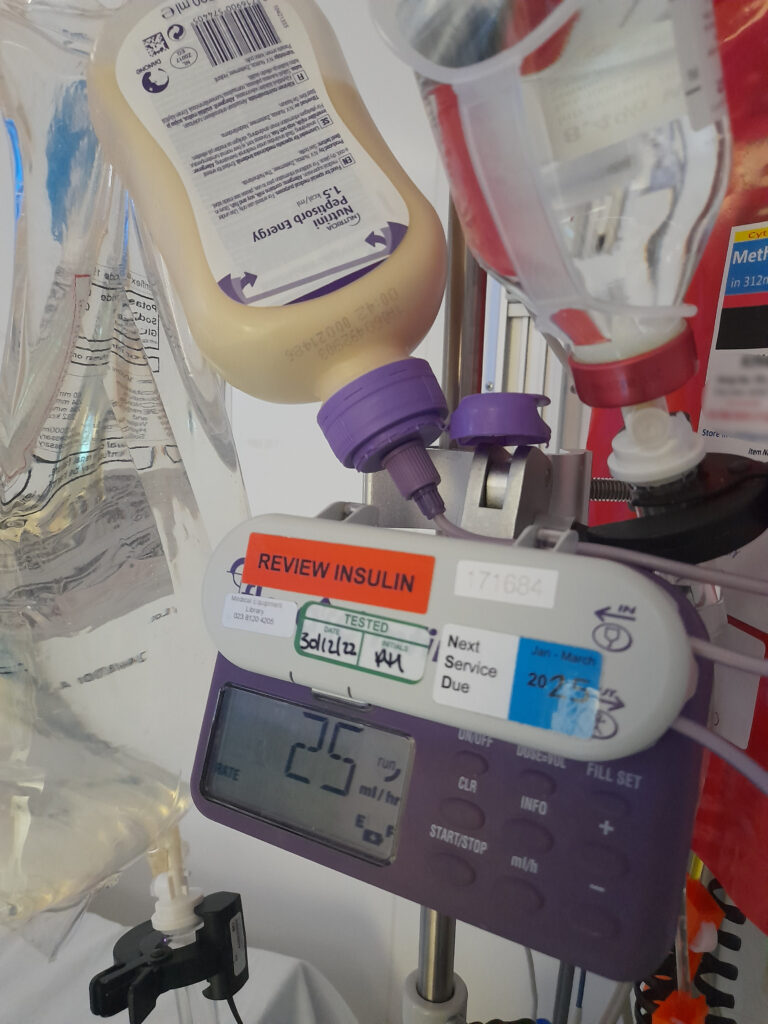
He went on the fluids overnight and they kept testing his wee. He also had to have his lumbar puncture the following morning and be put to sleep to have the methotrexate administered that way as well. And then they started the HD MTX a few hours after when he was ready to start. He was having so many things at once and he had to have multiple lumens plugged into his wiggly.
The HD MTX has to be done over 24 hours slowly, as it’s a high dose. The nurses told Christian they have to check the flow rates every 6 hours of the drug going into him, but didn’t explain why. They didn’t come in 6 hours and when Christian was chasing it up they came an hour and 15 minutes later, so Christian was really panicking and worrying Chester may be getting too much of the chemo. Finally, someone explained it to Christian and it turns out they just check the flow rate as the whole dose has to be used in 24 hours, so they need to make sure it’s running on time.
That was a very stressful night for Christian and could have been avoided if it had all been explained clearly beforehand, and we had been told exactly how it all worked and what was happening. Luckily we know for next time.
Chester still had to remain on the fluids to keep his hydration and PH levels up. They also give sodium bicarbonate to help with this. He has to have so much fluid as they need to help the body flush out the chemo. It cannot stay in the body too long as it would be dangerous and could cause serious problems. The quicker it’s also flushed out, the less chance there is to damage Chester’s kidneys, as HD MTX has a chance of doing that.

Chester absolutely smashed it! They checked his bloods every 6 hours after the 24-hour dose, and the levels of MTX were dropping very quickly, which was great. They also gave leucovorin (folinic acid) which helps decrease the toxic effects of the drug.
So Chester was admitted on Monday and technically would have been allowed home on Thursday morning, but that did not go to plan!;

1. Own Medicine
When we got to the hospital they asked if we had brought our own medication. We didn’t know we had to bring it and no one had told us.
After speaking to our clinical nurse specialist (CNS) she said it’s easier if we can remember to bring our own chemo meds that he’s on that cycle, like his imatinib and mercaptopurine. This is because we have our dispensed amount from the pharmacy each phase.
But she said it wasn’t a problem if we did forget them, as they could get it all for us when we were there if needed. Some nurses however were making a big deal out of it, even though we were unaware of having to take our own stuff. At least we know for next time!
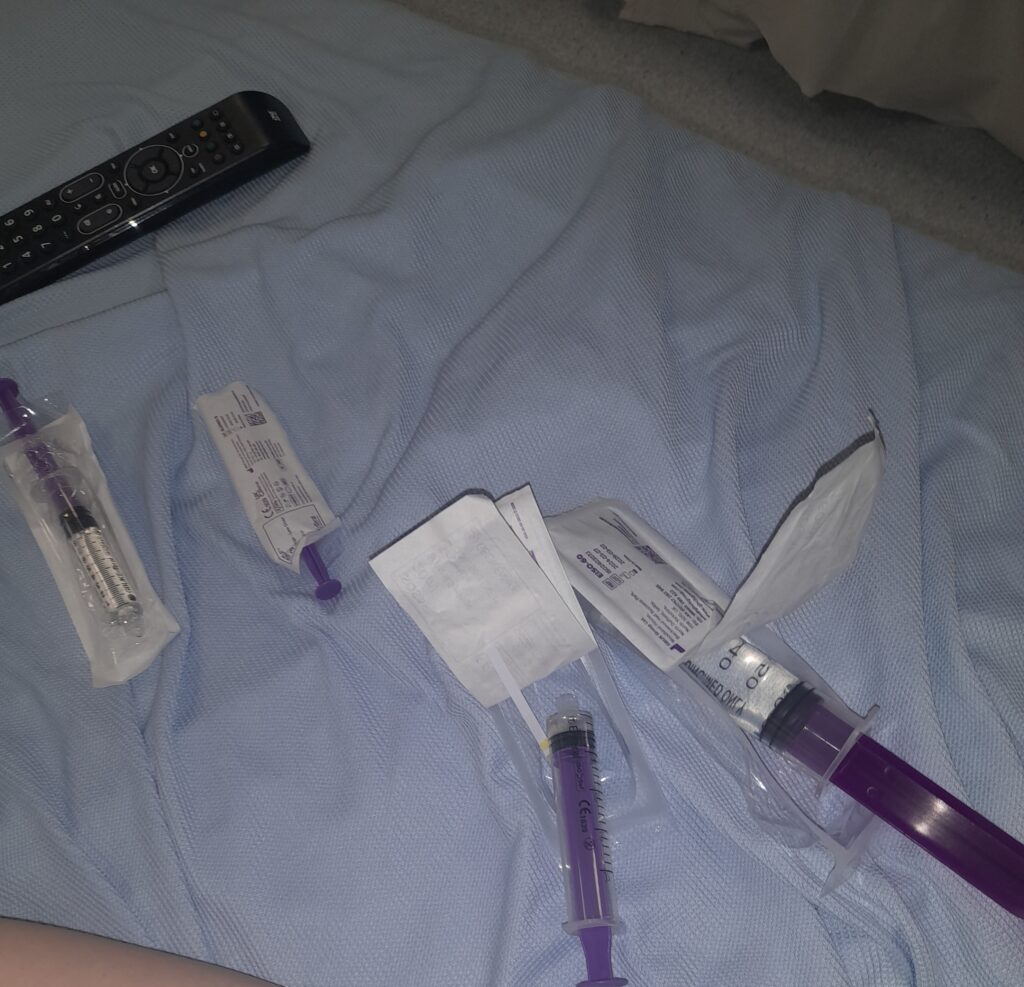
The other thing we did not expect was having to give Chester his medication when in the hospital. The nurses said that Christian had to give the chemo medication that we do at home down the tube ourselves while staying in the ward. Christian does this at home, but we are very new to it all and quite new to the NG tube, and we never actually get shown how to do each different chemo medicine and only guess that we are doing it correctly.

Also, the room was very small, and instead of bringing the correct amount that Chester needed, they were just bringing in the whole bottle of Mercaptopurine and the whole box of Imatinib. So Christian had to measure it all out in the small room and was doing it on top of the hazardous waste bin in the room. Not very hygienic at all! Sometimes they gave him a tray and other times they didn’t.
The nurses were administering Chester the other meds like his anti-sickness and antibiotics etc, However, towards the end of the week they were just bringing in syringes in their pockets and putting them on Chester’s bed for Christian to do.
The meds also need to be flushed after with clean water, but as the week progressed and Christian was being left to it, he wasn’t given clean water so had to use the drinking water jug. Then he didn’t have much himself to drink!

I swapped with Christian on Wednesday night to give him a break. The nurses had to do all the medicine for me as I wasn’t confident doing it through the tube. This is because I was very pregnant when Chester got the NG tube, so Christian had done it most of the time since Aurora was born and I haven’t done it much. We have our designated jobs to help share the care and get us through!
But when we swapped back again towards the weekend the nurses stopped helping and left Christian to it again. He spoke to our CNS and a couple of nurses in charge and said he was getting too overwhelmed with everything going on, having to make up the chemo on the bin, and then being constantly given different syringes throughout the day and not always knowing what was in them. We have also never done mercaptopurine in liquid, and they didn’t show us how and just left him with the bottle. Each medicine is different and some can be given quickly and some have to be given slowly.
So for the last nights that Christian stayed, they did do it for him. But asked him why he wasn’t doing it and weren’t particularly happy about it. One of the nurses said they have to be trained for years to give chemo, but we as parents like all the other parents have to do it after a couple of days and are not shown how to give each medicine.
We also had to change the dosage of Chester’s imatinib again. It was recalculated on his weight the last time we went in for a lumbar puncture, even though we told them they were using the wrong weight to calculate it. But they upped his dose to 3 a day. But when we went in to start his chemo for this phase, we were told by the pharmacist it needed to go back down to 2 one day, and 3 the next because of his weight!
Chester also has to have antibiotics every weekend called Co-trimoxazole to protect from pneumonia and fungal infections. This is given to everyone on the ward and at home with Leukemia, but they forgot to give it to him Saturday morning. I had to press the buzzer and ask, then wait an hour to be told he hadn’t been given it like he should have. The excuse was that they weren’t expecting him to be there over the weekend so it hadn’t been prescribed yet! But they knew Friday that he would be there until at least Saturday evening.
2. C-Diff
Unfortunately, Chester got a bad tummy on the Monday evening on day 1 and had bad diarrhea. Christian kept telling the nurses but they weren’t concerned.
It went on for two days and Chester had it really bad and stopped eating altogether because his tummy hurt and he felt rubbish from the 24-hour chemo.
When Chester is admitted to the hospital he has to go to the toilet into a bed pan that sits in the loo, so the staff can monitor his urine and kidneys and help monitor his fluid input and output. Then you have to take it to the dirty utility room. Christian asked the staff if they wanted a sample of his poo but they said no it’s fine.
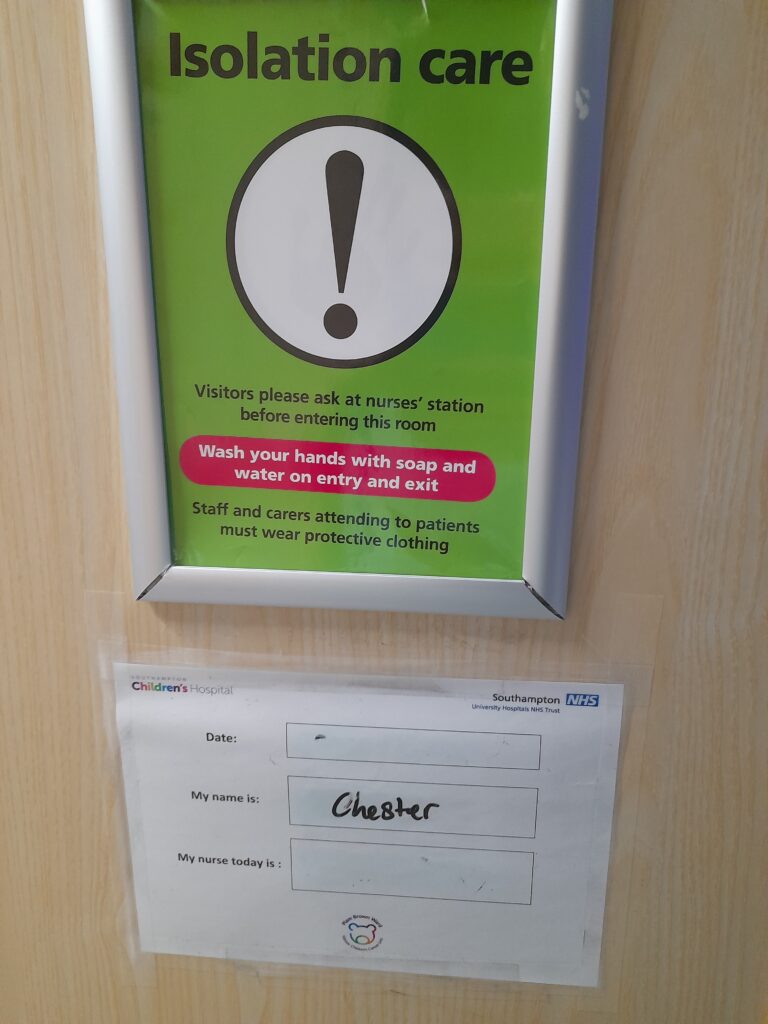
After 2 days the nurses changed over and they decided that Christian and Chester shouldn’t be wandering around and going into communal areas such as the playroom and kitchen, in case Chester had a bug. So they had to isolate and not leave the room. But they said Christian could still go into the dirty utility room to take in the bedpans.
This then made everything more difficult because Chester wasn’t eating much at all, but the only thing he would have was his own yogurts and lots of milk. He didn’t like the hospital food at all! But because they were isolated and not allowed in the kitchen, Christian couldn’t go and get it all when Chester was all of a sudden really thirsty or decided he wanted to try and eat.
The boys were told to press the buzzer for help. But the nurses were sometimes taking 30-40 minutes to arrive, or not at all.
They then decided to ask for a stool sample which was tested quite quickly and turned out Chester had C-diff (Clostridium difficile). This is a bowel infection that needs to be treated with antibiotics. It’s very common when being treated with chemo as the meds strip the gut, but also very contagious as it’s bacterial.
They then decided that Christian could not also go into the dirty utility room because of what Chester had. They said they would collect the bedpans each time Chester had gone to the loo. Because Chester was going quite regularly we would have to press the buzzer for them to collect it as the smell was making Chester feel sick. But at some points, there were 2 or 3 lined up in the tiny bathroom, as they either wouldn’t respond to the buzzer or said they would take them and forget or not come back!

Chester was still on track to come home by Thursday but then ended up with lots of blood in his stools. Again they weren’t worried, but we were concerned so asked to see a consultant. Finally, when we got one, they said it’s normal for c-diff. However, we weren’t allowed home for the next few days until it improved! We just didn’t know what was going on and were always going around in circles.
3. Temperature
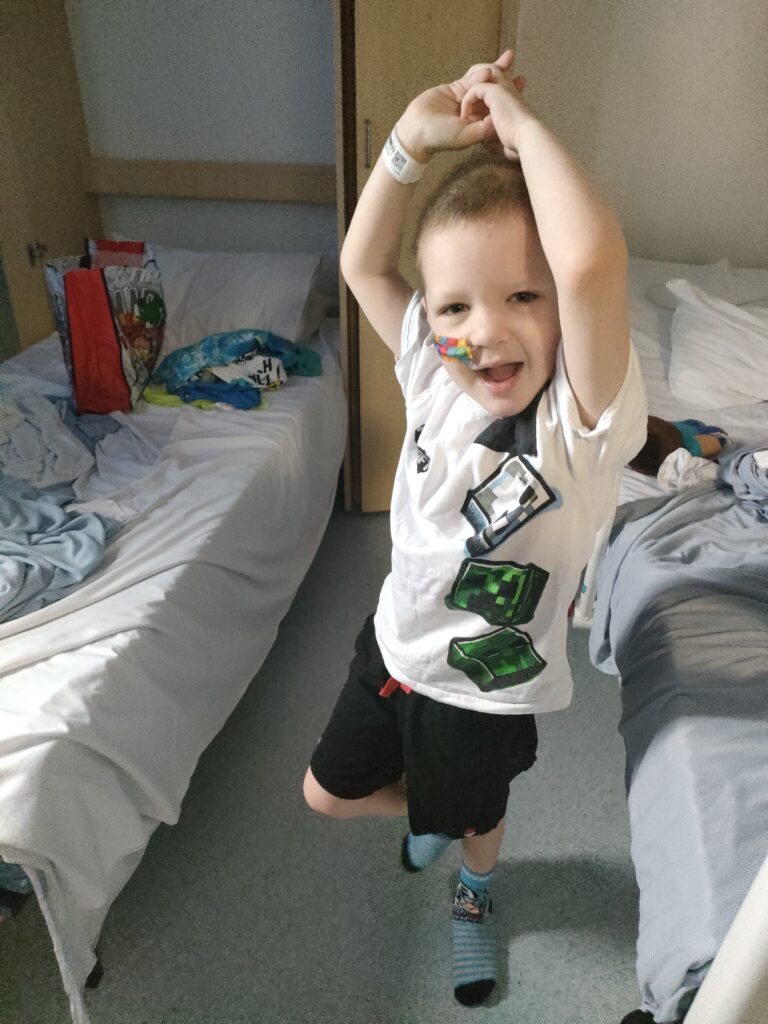
Towards the end of our stay, Chester spiked a temperature. But he was not too bad in himself and was feeling OK considering everything else.
If he has a temperature at home we have to get him seen within the hour to be checked and be given antibiotics. As he is immunocompromised, any small thing can be serious to him. His bloods then get sent off and they send some to the lab to grow cultures, to see if anything bacterial grows. It all gets tested, especially for important things like septicemia and sepsis.

So they sent his off and the results came back. His cultures were growing something but they thought it was a contaminant. They had to be done again and we had to wait on the results the following day, to see if Chester needed to be sent home with different antibiotics.
We waited all day Sunday for the results, to then be discharged at 5 pm (conveniently before they would have to give Chester his evening chemo), and said the results never came! We still actually never got the results at home a week later, so we are assuming that they were OK. We did ask community nurses to check for us and they never got an answer either.
4. Isolation & Food
So as I mentioned above, Christian and Chester were isolated to the room through the week after they decided his having diarrhea could be a tummy bug and be contagious. As everyone else on the ward is also immunocompromised then it makes sense. When I swapped over halfway through the week I also had to isolate in the room with Chester.
So we were not allowed in the parent’s kitchen and communal family room. They also decided later on that we could no longer go into the dirty utility room.
However, it was horrible as we were stuck in the four walls of the room on our own. None of the usual charity ladies could come in and visit us, and the nurses didn’t want to come in too often as they had to put a gown and gloves on each time.

We had to press the buzzer anytime we needed anything, and we understand how busy the staff are. But sometimes it was taking a long time for anyone to come. So if Chester was really thirsty or hungry, we had to wait for them to get us milk for him.
We also didn’t want to bother the nurses by asking them for water and food for ourselves as they were really busy and often went without. We also didn’t want to ask as we felt like we were being a nuisance, and sometimes just asking for a fresh jug of water came with an eye roll or a huff. But it wasn’t our fault we were not allowed to leave the room while staying.
On the first day of isolation, poor Christian went without food all day, and when chatting with the cleaner she said when in isolation you should be offered meals! But no one had offered him any at all. Luckily they found him a sandwich in the fridge but that’s all he had that day. Thankfully the lovely cleaner and also one of the charity ladies went and had a word with the nurses, so the next few days we were offered food and ordered off the same menu as Chester.
As I mentioned above, the bedpans were sometimes stacking up. We needed new bedsheets on several occasions as Chester had either been sick on them or Christian had spilled chemo meds on them while having to make it in the room, and they were taking over an hour to bring new ones.
Chester had been going off his food for a while, and for the 3 weeks before this chemo, he had barely been eating anything and just wanted gingerbread men and ginger biscuits. Probably to help his nausea. We were telling the community nurses and a few consultants, but no one was interested and kept saying it was fine as long as he was grazing! But we could see he had lost weight. And grazing on biscuits and yogurts is not enough.
When he went in for treatment they realized he had lost nearly half a stone, but we had to push to see the dietician. She didn’t come in when she was supposed to and Christian had to chase up and push to see her all day. When she spoke with Christian she said Chester had lost too much and that we needed to get him on feeds through his tube. So now we have a pump for home and also a load of ready-made drinks and yogurts that he can drink/eat or be pushed through his tube. I will write more about this in a post about his ng tube.

5. Side Effects
Chester also had an allergic reaction to one of his medications, possibly one of the new anti-sickness medicines they gave him. He came up red and spotty all over and had hives all over. It was quite scary and they gave him some Piriton (anti-histamine) which helped bring it down.

He was also extremely tired after the 24 high-dose meds. And stopped eating all week because of this stuff and also because of his tummy bug.
This also caused a really sore mouth for a few days and a couple of ulcers.

After a nightmare week in the hospital, the following 2 weeks have been pretty easygoing. We have just chilled at home while Chester recovered, and he has been playing with his sisters. Willow had missed him so much!

On week 2 (the week after the hospital stay) he had nothing booked in for the week apart from taking his Imatinib still daily, and also the new mercaptopurine daily. The nurses came around to check his blood and his blood counts had dropped, which is meant to happen. As his neutrophils dropped to nearly 0 he had to pause his mercaptopurine for a while, to let his body recover. But they know the chemo has worked as all his blood counts had dropped in his bone marrow.
He was due back into the hospital again this week (week 3) for another round of high-dose methotrexate. His bloods were still too low at the beginning of the week and his neutrophils were still under 0.5, but they were climbing through the week. The nurse came out to do bloods yesterday and they were up at 0.7 so high enough to go back into the hospital next Monday for the next round.

So overall it was a bit of a nightmare week in the hospital. But we know for next time what should be happening and what to expect, and hopefully no bugs! Christian did speak to the Matron in charge and I spoke to our CNS and they said we will make sure it is better next time, and took our concerns on board. They also said we do not need to administer the chemo ourselves in the room, which has taken a big weight off our shoulders.
It has been nice the last couple of weeks just chilling at home while Chester’s body recovers and all being together. And Chester and Willow have had great fun playing together.
