Toward the end of the induction treatment for Chester’s leukaemia, I mentioned briefly how Chester had to get an NG tube fitted.
The reason for this is that he started to refuse to take his Imatinib tablets as he said they smelt horrible and did not taste nice!

What is an NG tube?
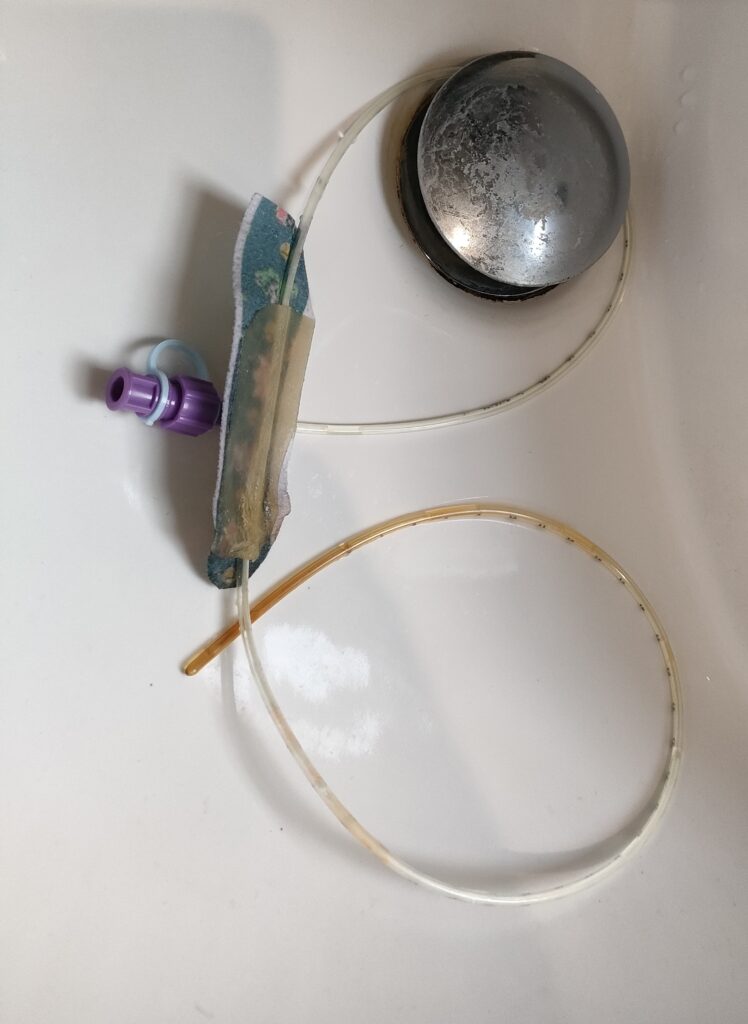
A Nasogastric tube (NG Tube) is a thin plastic tube that is inserted through one of your nostrils, down your throat, and into your stomach.
This then allows us to be able to put water, food, and medication through the tube and straight into Chester’s stomach meaning he does not need to take tablets anymore.
We were told by a lot of the doctors and nurses that Chester had done well so far and that a lot of children get the tube straight away. And most children his age do not take tablets!
They said it was pretty inevitable for children on chemo to have an NG tube. And unfortunately, all the children they have come across that have to take Imatanib (although rare so a very low amount), have a tube just for that one medication also.

Why did Chester get an NG tube?
Chester had been doing so well taking tablets since his diagnosis. But because certain medications were making him really nauseous and physically sick, he then began to struggle with taking his tablets.
We do give him anti-sickness medicine, as nausea can be a side effect of Imatanib. But the chemo he was having in the last 4 weeks of the induction was so strong that it wasn’t even helping at all, and he just couldn’t keep much down.
Because the Amarox imatinib’s had a coating, they left a residue on his tongue and started dissolving as soon as he put them in his mouth. Then making the water he drinks after to wash them down “taste yucky” (in Chester’s own words).

So he then began to refuse to take them and it was a real chore getting him to take the Imatinib. He had developed a fear of taking them because he thought they would “make him sick all over the sofa and everywhere else”.
After a few days of trying to get Chester to take his tablets (starting anywhere from 7 am to 10 pm), we had to contact his treatment hospital for advice on what we could do next. Unfortunately for Chester, he has to take Imatinib every day because that is the one medicine that targets the Philidelphia chromosome he has. Without it, his mutation of Leukaemia can be very tricky to treat and get rid of completely. So we started to stress a lot as these were the ones he was struggling to take.
He was still OK taking his anti-sickness tablets, and his weekend antibiotics, just not these as they tasted and smelt so bad, which I agree with as they do smell horrible.
We tried the nice approach and the firm approach with Chester. We then resorted to bribery. But it got to a point where he stopped taking them at all. Originally it was taking all day, then he became so scared he just couldn’t do it. But he had kept being sick after taking them because of the taste.
It had begun to stress us all out at home and we were becoming very tired and quite ill with stress and worry ourselves. After a bit of chasing as no one seemed to be interested in helping us, they then managed to come up with another branded imatinib called Santoz. These tablets are apparently tasteless, nonsmelling, and have no shell coating. So these sounded ideal for Chester. Ao Christian drove the 60-mile round trip to collect the tablets straight away.

Unfortunately, after Christian returned with the new immatinib tablets Chester still refused to take these despite us showing him they were new and do not smell. We then had the community nurse come out the next day to see if she could get him to try the new tablets, but after an hour she had no joy. We thought it would work because he knew the foul smell and taste had gone, and he really likes the community nurses, but he just could not psychologically get over that fear.
The discussion of having Chester a ng tube fitted began and we all decided that this would be the best route, as it was becoming too stressful for Chester and us trying to get him to take the tablets and we couldn’t go on like that. He just became too scared to take them as he thought he was going to be sick like he was on the previous tablets. He had also missed a couple of doses so we really needed him to take them.
We had also tried all the tricks in the book that book like dissolving them in water, apple juice, and nicer-tasting drinks. Also putting them in yoghurts and other food, but he just couldn’t do it anymore.
How was the NG tube fitted?
Later that day Christian took Chester to our local hospital to have the ng tube fitted. The nurse gave Chester another chance and was very good and patient with him, allowing him to try to take his tablets before fitting the tube. But even being in the hospital and having one more chance, he was still too scared and not wanting to try it. He was literally shaking when he tried to take them.

They measured the tube to the right length. Then Christian and the nurses had to hold Chester while the tube was being fitted, due to it being uncomfortable as it went in. He had to do this awake and did not have anything to take the edge off.
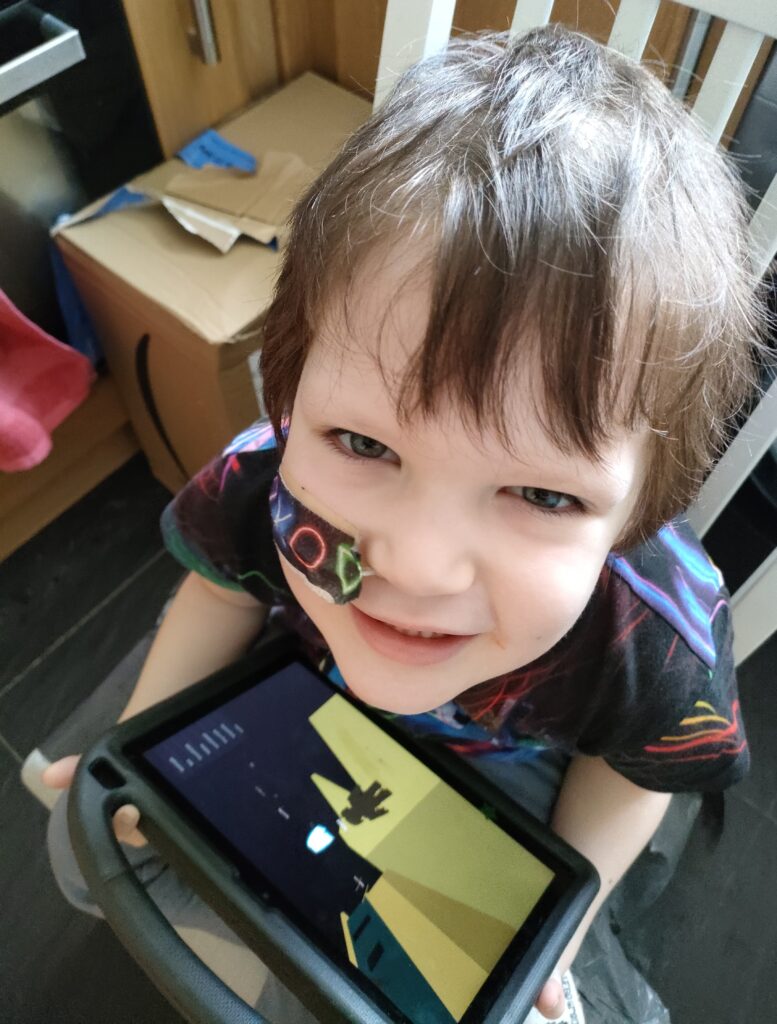
After the tube was in the right place, it was secured to his cheek with adhesive tape. But there are cool ones he can choose from that make him feel better about it, like his PlayStation and Mario ones.

The procedure usually isn’t painful, but it can be uncomfortable for a short time. But Chester said it did hurt him.
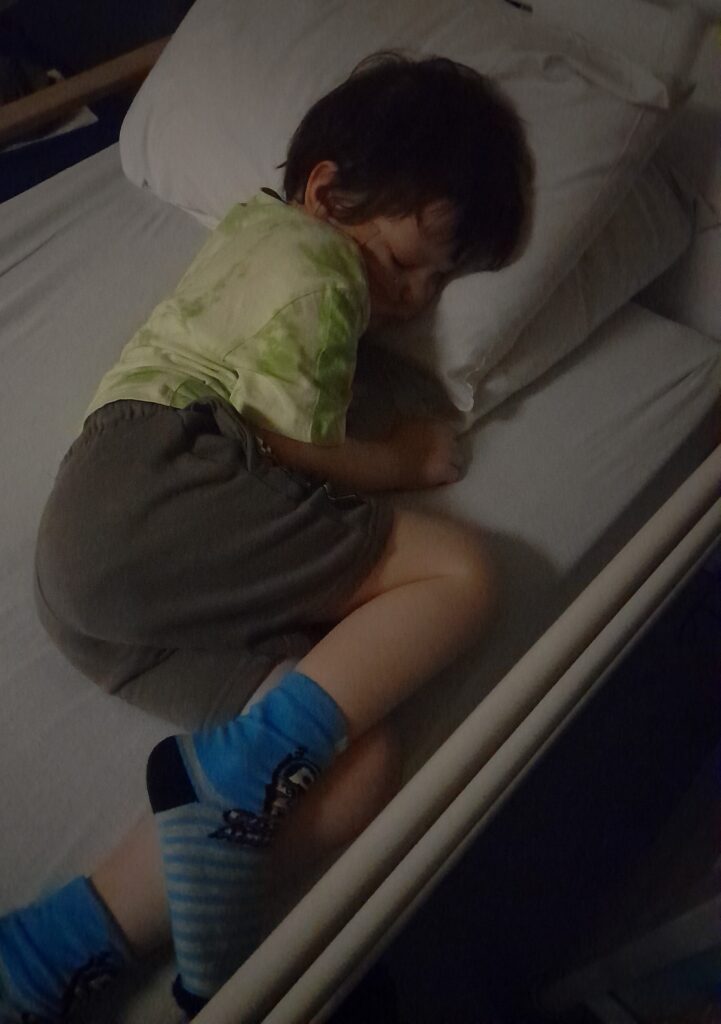
Once the tube was fitted Chester was very emotional and not impressed and wanted it taken out. He was so worked up and hysterical that the nurses were struggling to keep the tube stuck to his face, and were worried it was just going to come out!
In the end, the nurses and Christian took Chester into the outside play area where Chester had a play on some drums and a ball and calmed down.

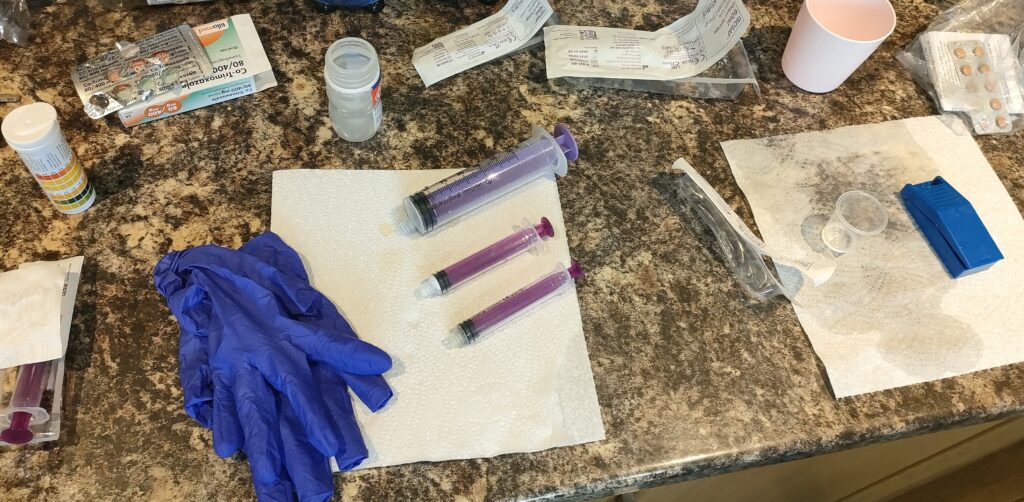
Myself and Christian had to stay in the hospital for a few days so we could be shown how to use the NG tube to get the medication into Chester, as it involves flushing the tube, checking his stomach acid (aspirate) with pH strips to ensure it is in the correct position, and ensure the tape that holds the tube in place is also okay.
Medication through an NG Tube
After a few days, Chester was free to come home and the stress of trying to get him to take tablets was removed. However, trying to dissolve the imatinib tablets was the next task as this takes a very long time meaning Christian is stuck in our kitchen for 30 minutes mixing and dissolving the tablets.
Chester then decided that he wanted a break from all tablets, as he realized through the tube he didn’t have to do anything and didn’t feel or taste anything.
So we also had to try and dissolve the PCP tablets on the weekend, and that was tricky as they do not dissolve properly and leave a load of powder/residue in the bottom. Christian ended up blocking Chester’s tube but managed to flush it by carefully doing a pumping action with water and flushing it through. Luckily we now have a liquid version.
We also now have a problem with storage as we have boxes of syringes and getting through a lot!
This is also then causing a lot of waste and we are having to use a lot of Dettol wipes and kitchen roll to clean up and wipe down the sides after doing the medication. It is very messy compared to tablets as you need to ensure you have no air in the end of the tube so you have to push the air out and get medicine everywhere.

With all the extra waste we had to ask the council for a bigger bin and extra recycle bin!
It is quite a lot of mess and things to sort and very time-consuming when he has to take more than one medicine at once, which will happen a lot throughout his treatment.
How long does the tube last?
We were told it could last up to 3 months possibly but annoyingly Chester was sick one evening and it came out. They aren’t permanent and if Chester does want to take tablets again he can have it removed anytime. But for now, he said he is on a break from tablets.
But they can come out very easily. So when he was sick which does still happen because of his nausea and Imatinib, his tube came out. So the community nurse came out and put a new one in at home.
He was happy to have a replacement and was prepared for it, but Christian still had to hold him while it was done as it wasn’t very comfy. And he was still quite distressed after. But the nurse gave him his usual stickers after being brave, so he was happy with his superhero stickers!
So overall having the tube fitted has made our lives much easier. But the only thing now is how time-consuming doing medication through the ng tube is, such as his anti-sickness in the morning and imatinib in the evening, then co-trixamole on weekends.