Just a little catch-up on Chester this week — same old routine as before, really, but this time around he had his lumbar puncture (LP) scheduled the day after his monthly vincristine, so it ended up being back-to-back with our usual visit to the local chemo clinic.

So we took Chester into his local hospital for his vincristine. Everything went smoothly, except they didn’t have his ondansetron, which we were told would be there. That meant we were left having to cut it pretty close with what we had left until the community nurse’s next visit. In clinic, she told Christian she was about to go away for two weeks, but we worked out we should just about have enough if she came round on the Tuesday like she said, once she was back from annual leave. We could have picked up the anti-sickness from the pharmacy, but honestly, we didn’t want to go in with all the other ill patients — especially not with Chester. The last thing we wanted was to end up in hospital for a few nights and Chester to have unnecessary medication to fight an infection, just because we caught something in the pharmacy waiting area.
Getting ondansetron is a bit of a saga sometimes. We always ask the nurse to bring it out on their weekly visits. We were due a top-up the week before but only got four bottles (as usual, both oncology doctors at our local were off at the same time — seems to happen all the time! — and pharmacy could only give us so much without their say-so). We were told we could get the rest when we came into clinic the following week, but when we went in, the nurse didn’t have it for us and said we’d have to wait another three weeks until she was back, or maybe the cover nurse could bring it out — but she wasn’t sure.
So as I said above, we worked out we’d just about have enough to last until she got back. For the next two weeks, the cover nurse visited, but nothing was ever mentioned about it. Then this week, I asked again if she had any ondansetron and she said yes, she was bringing it out. But then a different nurse knocked on our door and dropped it off, saying she’d actually picked it up for us the previous week but just forgot to give it to us! So she’d had it all along but forgot. Honestly, it’s always like this: you have to ask for something, then remind them several times, and just hope it eventually turns up.
We are grateful though — it was really kind of the other nurse to pick it up for us in the first place. Most of the delays with prescriptions are usually down to pharmacy issues or the consultants taking ages to write them.
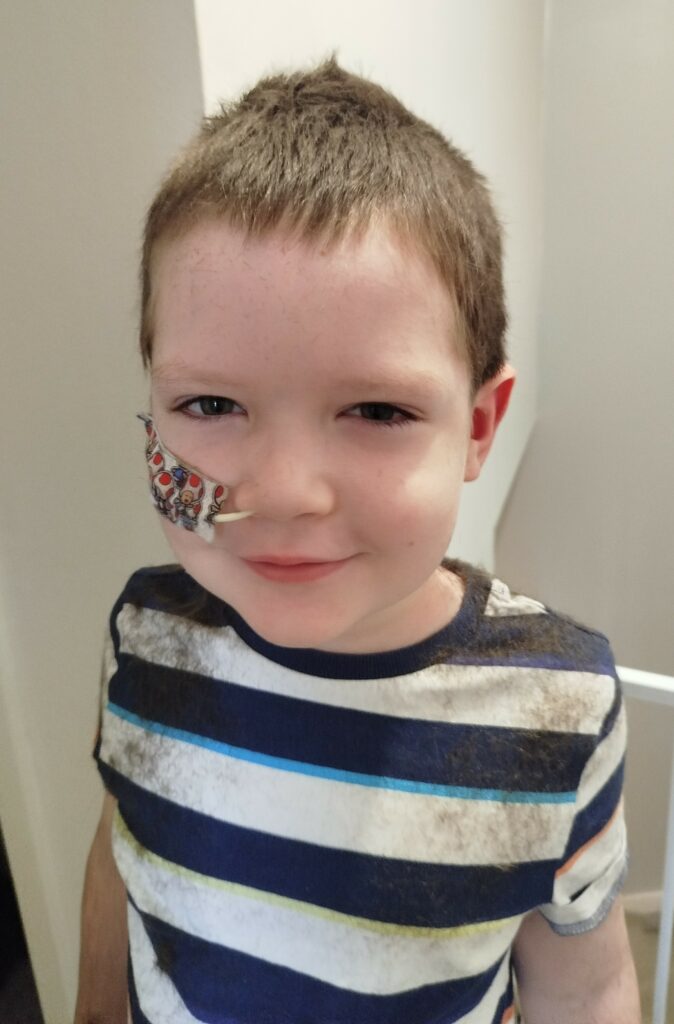
If you’ve been following along, you’ll know all about the NG tube saga recently — with the hospital saying they no longer routinely change them, which has been a massive stress and worry for us. So we’d been on edge all morning, not knowing whether Chester’s NG tube change would actually go ahead during his LP.
They did end up changing it in the end, but when we first arrived, no one seemed sure whether it was happening or not. The nurses checked with us and said, “Does his NG tube need changing today?” — so at least they’d made a note of it. But they also said they couldn’t confirm anything yet because the anaesthetists weren’t in, and the decision was down to them. So once again, we were left waiting without being able to tell Chester, which just adds more stress. We only found out it was going ahead as we were being called in, so we had to tell Chester at the very last minute. Not ideal when we try to give him a bit of time to mentally prepare and make him feel more comfortable about it.

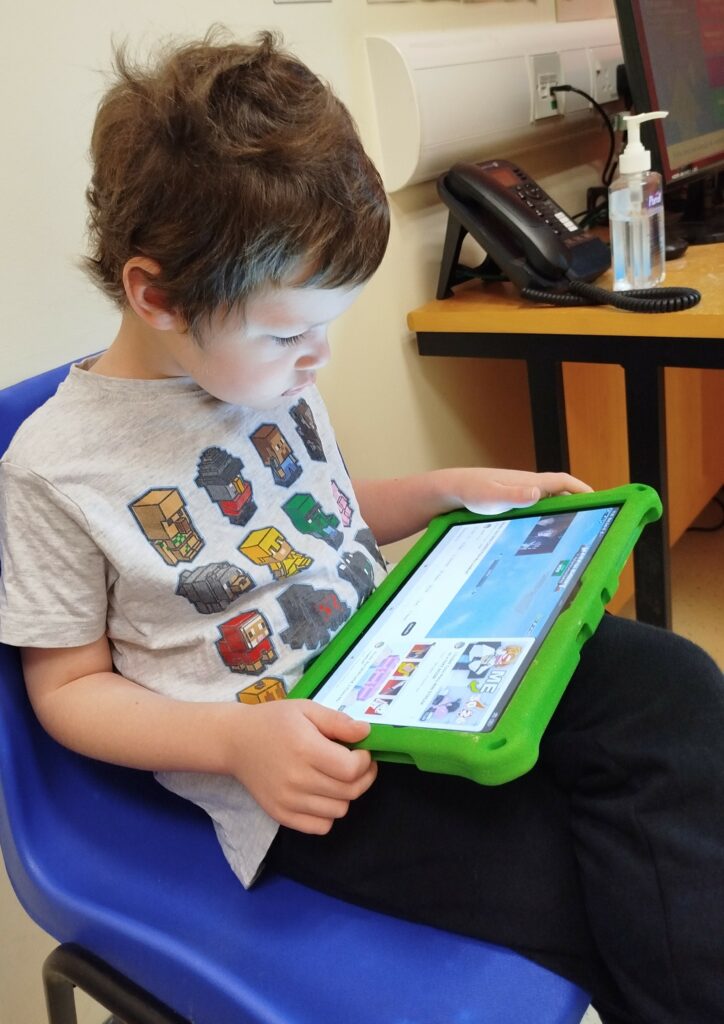
When we arrived at the ward, we were told the list was short that day, which was apparently why they decided to change his NG tube. But even with only five kids on the list, we still ended up waiting hours for Chester to go in. When Christian chased it up, he got a similar response from the receptionist as he has before. He simply asked how much longer it might be because Chester was starting to get emotional, and she replied, “They’re all getting emotional.” Christian explained that Chester was on steroids, and she just said, “Well, they’re all on steroids,” instead of actually bothering to check. All it would have taken was a bit of empathy — it’s such a stressful time for the kids and the parents, but apparently that’s too much to ask.
In the end, we got called in late in the day, and it honestly felt like we’d been left until late just because they had the “extra” two-minute job of changing his tube as well.
The pattern has become pretty clear now — it doesn’t seem to matter whether we arrive early or a bit later, whether Chester’s in maintenance or not, he always ends up being seen really late. And honestly, it feels unfair. Most times he has an LP, he’s on edge, on steroids, starving, thirsty, and very emotional. They say they decide the order based on who arrives first and what medication the kids are on, but on several occasions Chester has still ended up being the last one in the recovery room. At this point, we are starting to think it doesn’t really matter what time you get there. Not to mention, the anaesthetists never seem to turn up until later anyway, so I don’t know why they insist everyone — including consultants — comes in for 8.30am.

Chester tried to play his little game again where he sees how long he can stay awake while they’re putting him to sleep. He managed around 15 seconds this time, which was very impressive! We like turning it into a game to make the whole thing a bit more fun and less scary for him. Even so, he still gets nervous about it — especially because his back always hurts for a few days afterwards, and he knows what’s coming.
They also put in a different type of NG tube this time, so hopefully this one will last a bit longer than the previous ones — fingers crossed!
Chester has been saying he’s getting pain in his hips on both sides, pain in both arms under his armpits (which moves around when he raises or lowers his arms), and pain in both legs. He also says it hurts when he sits down. His back has been hurting too, but that could be from his LP, as they stick the needle into his back for that. Chester stopped taking steroids on a Monday, and the hospital say the pain is either related to the medication or his muscle strength — but we are not so sure it’s just that. He’s always complaining about aching and being in pain, so it feels like more than just weak muscles. The hospital don’t seem too concerned though; all they ever really ask is whether he’s taking morphine for the pain. Chester refuses to take it and just says he’ll deal with it.
He’s also still really struggling with the smell and even the look of certain foods. For example, he doesn’t like the look of Ritz crackers anymore because they make him feel sick. It’s crazy how much the chemo has affected all of Chester’s senses.

This week and last, Chester really hasn’t felt up for doing much. He’s spent a lot of time laid up in bed, not feeling great, just trying to rest and get through the days. Some days he’s just completely wiped out, between the pain, sickness, and everything else the treatment throws at him. Even so, he’s still doing amazingly well — he’s such a tough little boy and keeps going, even when he’s not feeling his best.
They also gave us an adult bottle of co-trimoxazole this time, which was basically double the dosage of what Chester usually has. Luckily, we always check and read the dosage labels every single time, and never just assume it’ll be the same — even though it usually has been for well over a year.
To be fair, they do occasionally change his doses if he’s grown a bit taller or gained some weight, but it’s so confusing. So if we finish a bottle, like his mercaptopurine for example, and move onto the next — suddenly the dose amount is different. Apparently, they work it out based on a three or four-month weight average, which doesn’t help make things any clearer!
We were told that the nurse would always check with us in clinic when she hands over his monthly meds, just in case the doses or amounts have changed — so we can discard the old bottle and switch straight to the new one. But she’s yet to actually do that.
Just like before, this week we didn’t get Chester’s blood results back until late the next day. His bloods were taken yesterday at 3 pm, and by midday today we still hadn’t heard anything, so I had to chase it up myself. That’s when we finally found out he’s still on a chemo hold for another week. Funnily enough the last 2 weeks when we had the other community nurse covering, we got the blood results both times within a couple of hours!

If you read our last post, you’ll know that Chester’s been struggling with hot flushes and night sweats for a while now — and unfortunately, it’s still ongoing. Every night for the past three weeks, he’s woken up at least once, sometimes absolutely dripping with sweat. His pillow and sheets are often wet, and his hair can be completely soaked through. He always comes into our room saying he’s hot and thirsty, so we end up going downstairs to get him milk — water makes him sick, so milk is the only option. As you can imagine, we’re all absolutely shattered from the constant broken sleep.
We’ve mentioned these symptoms to the community nurses several times, but their response is always something along the lines of “it’s just the steroids,” even though he hasn’t been on steroids for three weeks now. We’ve also brought it up in clinic, but usually we just get vague answers like “keep an eye on it” or “it’s probably the chemo,” and no one ever properly explains whether it’s normal or something we should be worried about. Sometimes they don’t even answer — just give us a look. It honestly feels like there’s no point telling them about side effects anymore, because nothing ever seems to get followed up.
We actually mentioned the hot and cold flushes to Chester’s main oncologist months ago, and he said it could be thyroid-related, which they can test for, but to just keep an eye on it for now. We raised it again with our community nurse recently, and she’s said she’ll pass it on to the local oncology team at next week’s clinic, since it’s clearly not linked to steroids anymore. We’ll see what they say, but it’s been going on long enough now that it really should be looked into properly.

On top of that, Chester’s in his second week of a chemo hold because his blood counts randomly dropped really low, so his neutrophils and immunity are too low for daily oral chemo at the moment. Of course, he doesn’t get a full break — he still has to take his Imatinib every day — which hardly feels fair.
Apart from all the negative sides of everything — which, let’s be honest, always feels like a lot — Chester is still battling on through to get to the end. Maintenance was meant to feel more like “normal life,” but it’s really not easy, and it’s definitely not the version of normality we were promised at the start.
We also gave Chester a little haircut this week! His hair had grown really long and fluffy since he lost it all, and we’d been a bit nervous to cut it. But we thought maybe trimming it might help with him overheating at night (spoiler: it hasn’t). Chester wanted to wear sunglasses while we did it to stop the bits going in his eyes — he looked like a proper little rock star.

Even so, he keeps going. He’s been trying to do some drawing and Lego again, even though his aches mean he can only manage short bursts before needing a break, and walking has become more of a struggle lately too. But despite it all, he still finds reasons to smile when he can — and of course, to wind us up like only he can! He’s a little prank master, and those cheeky moments remind us just how strong and brilliant he really is.
