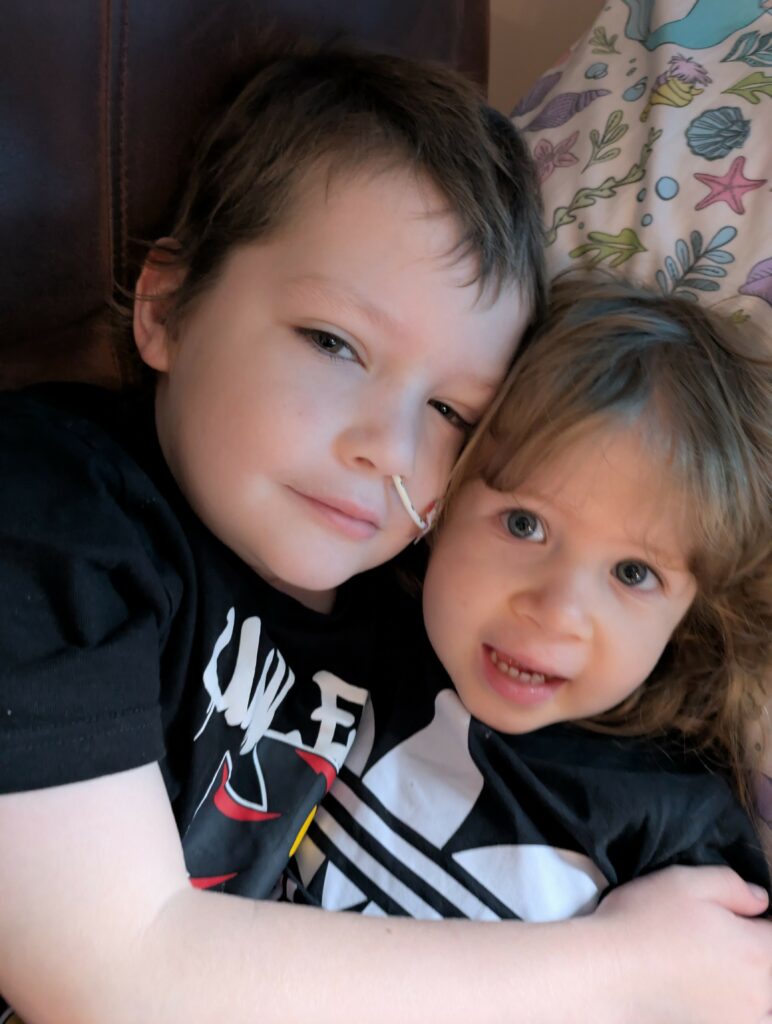
Chester hasn’t been too bad this week, though he’s still talking non-stop about the Lamborghini he went in (if you didn’t catch that post, you can read it here!).
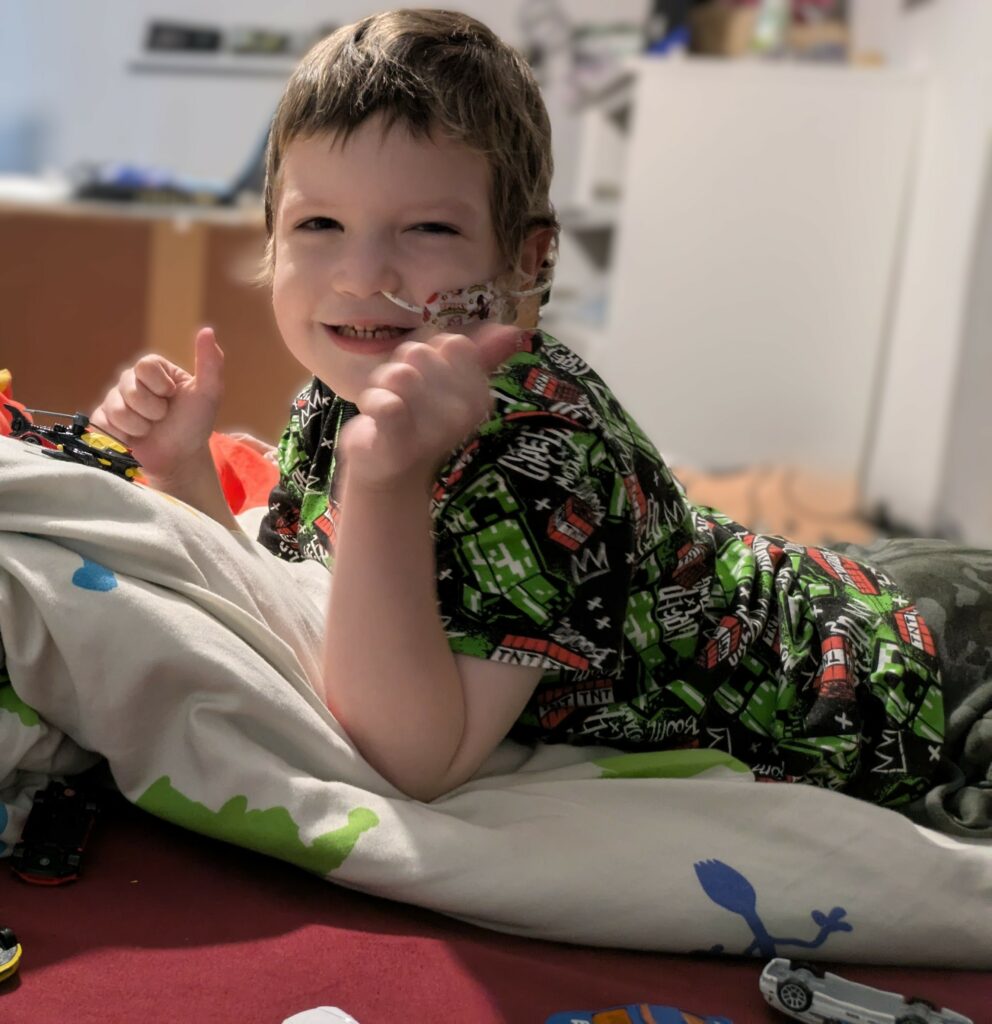
This week he’s been complaining a lot again about pain all around his body, mainly in his legs, but also in his arms. For example, he says he can’t draw for too long because it makes his arms ache, and even holding a packet of crisps hurts after a while — so he always rests things on his legs instead. Because of this, Chester has been spending a lot of time laid up in bed over the past few weeks.
I mentioned all of this to the consultant at our local treatment centre during our last appointment — all the aches, pains, not being able to draw, and needing to lay in bed — and her response was basically, “oh, it’ll just be because he hasn’t used his muscles much” and she said something about muscle memory or something similar. But the thing is, Chester has been using his muscles, and this aching has only got worse recently. It’s not the first time she’s given us a strange explanation, either. Before he was diagnosed, when he was getting really skinny and unwell, she kept saying it was a “mystery illness” she’d never seen before. First she said his muscles were inflamed, then she changed her mind and said they were wasting away — but looking back, he was losing weight because he was actually really ill and had leukaemia. She also told us his muscles were wasting just because he stopped moving his arms for about five days! And the most frustrating bit? This consultant turned out to be the “oncology specialist” at our local hospital, and she’s the one we still see at the monthly chemo clinic.
She also told us at the beginning that it might be “suspected arthritis,” which was then ruled out by ultrasound, but after that she just left us with a couple of hydrotherapy sessions and disappeared — we couldn’t get any proper follow-up or answers, no matter how much we chased. Even though Chester had a swelling on his spine that showed up on MRI and neck scans, they just said it wasn’t normal but didn’t look into it further, as they’d decided it was probably “arthritic or inflammatory,” and nothing to do with the pain all around his limbs.
It turns out, looking back at those MRI reports recently, there were also some suspected unusual shadows down his spine that might have been a clue — but we only found out about that now, months later. Then, two months after that first scan, when Chester finally had an MRI at the main treatment centre, the shadows down his spine were picked up straight away as abnormal and cancer was immediately suspected. It’s honestly hard not to wonder how much those shadows could have progressed in that time, considering how aggressive his leukaemia turned out to be. If they’d actually followed up properly, or done more scans like the original radiologist suggested, maybe we could have had a diagnosis earlier. Regardless, they should have at least followed up on his weird symptoms, the swelling, the shadow, the neurological signs, and the fact that they kept saying his bloods were “off” and not normal. But I’ll save that whole story for another post, as it’s honestly a saga all on its own.

We’ve always mentioned Chester being in pain, not drinking much, and still not eating properly. Most of the time it’s only little amounts, or he wants to eat chocolate or rubbish food. That said, he does sometimes try new things when he’s up for it — this week we even managed to get him to eat a little potato, Yorkshire pudding and gravy, and he’s back on the cheese and onion Hula Hoops. He is also eating strawberries everyday. But overall, he’s really not eating well. When we bring this up with the community nurse, they don’t seem to say much, and when we take Chester into hospital for his monthly chemo, they just say, “well, he’s on the same weight.” So it never seems to be a red flag. I can’t help thinking — surely him getting taller should count for something, not just the number on the scales?
This week and last, Chester has been feeling quite sick from the smell of food and even other random things in the house. All of a sudden, he’ll either leave the room until we get rid of the smell, or he’ll go upstairs — even though we can’t smell anything ourselves. Honestly, he’s got a nose like a sniffer dog at the minute! To be fair, he’s pretty much had this problem since the very start of treatment last April, but it seems to have ramped up again lately since maintenance began. Every time we mention it, though, no one really says much. The only response we ever get is, “are you giving him anti-sickness?” — which, of course, we are.
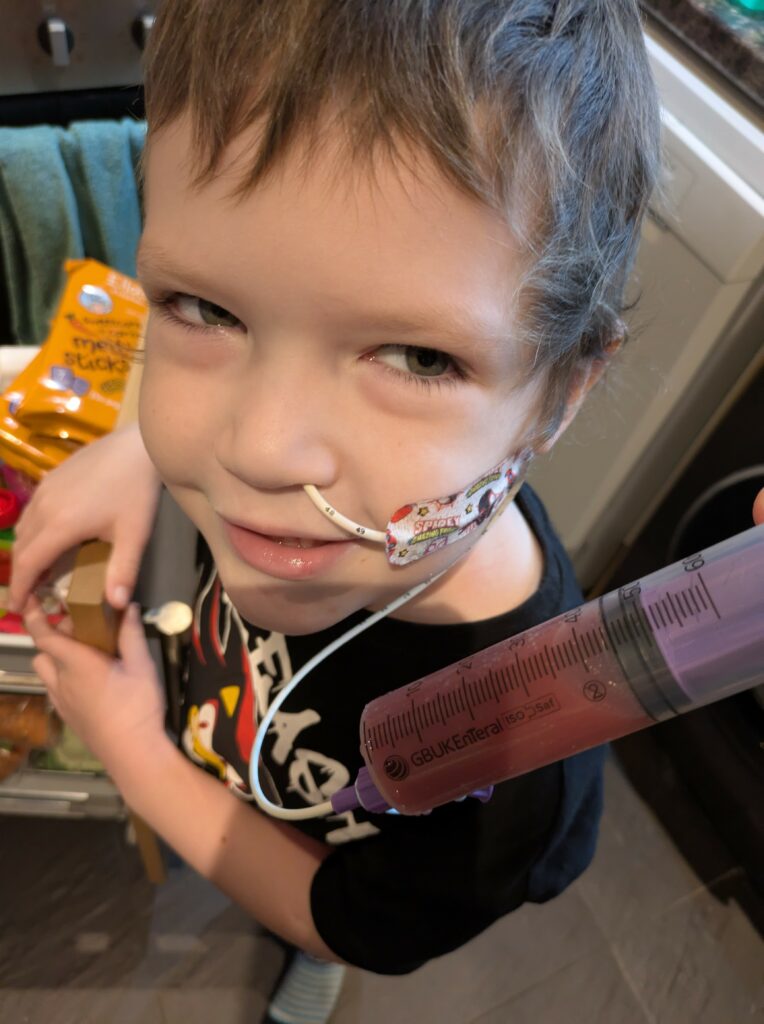
We found out that Chester’s bloods were low last week. They were taken on Thursday afternoon during his weekly community nurse visit (where they do his bloods and change his central line dressing — but not his NG tube dressing, because apparently “it’s not something they do,” so that’s left to us, which is always a bit stressful as we only got shown how to do it once or twice and we’re definitely not professionals). These weekly visits aren’t even on the same day each week — sometimes Tuesday, sometimes Wednesday, Thursday, or completely random times — which doesn’t help either. Back in intensive treatment, we’d always get the results back within an hour or two, but since starting maintenance we often don’t get them until the next day, sometimes even later.
The whole point of these weekly bloods — is to check if his counts have dropped too low, so they know whether to reduce his chemo to 50% or put him on a week’s hold. But because of the delay, by the time the results came through on Friday lunchtime, it was already too late. Christian had given Chester his full oral chemo on Thursday evening as usual, and then his full methotrexate dose on Friday morning at 10:30 — again, as we always do, and as the hospital know is routine — still with no results back. When the results finally landed, they said his neutrophils had dropped to 0.4 and that he was to stop all oral chemo for the week (except for imatinib, which he always has to take). I messaged back saying, “Oh, but we’ve just given him a full dose of methotrexate — is that ok?” and the nurse just said, “fine.”
Honestly, I don’t know if she even checked with his consultant or was just winging it by saying that. But really, we should have been told the day before, because he should never have had those extra doses in the first place. Back in intensive we’d always be told straight away if his bloods were low — but since starting maintenance, it feels like there isn’t the same urgency anymore, and that’s really worrying.
We saw the community nurse again yesterday to take this weeks bloods and told her about Chester’s pains, eating, and everything else like we always do. This time, though, Christian actually asked her if she passes this information on to the hospitals — because we’ve never seen her write any of it down. She basically said no, not really. She only passes things on to our local hospital, and even then she doesn’t write it down, she just remembers it in her head. Which, let’s be honest, is impossible to remember properly. She just said, “tell them next week when you’re in clinic.”
Christian then asked if the local hospital passes the information on to Chester’s main treatment hospital, and again she said no, not really. They do have a monthly oncology meeting, but it depends who’s there, so half the time it doesn’t even get passed on. This isn’t what we were told at the start — we were promised that everything would always be passed on to Chester’s main consultant so he was in the loop, but it really doesn’t feel that way now.
Christian also asked about reporting side effects for the trial, and again, she didn’t really have an answer. I even said, “so is there any point in us telling you anything then?” and the nurse just replied, “yes, but only if Chester gets weird symptoms or something out of the ordinary.” The problem is, no one ever tells us what counts as “out of the ordinary.” Chester being in pain every day — is that normal? Or is that something that should be reported? We’re left in the dark.
And as if all that wasn’t enough for one visit, while the nurse was changing Chester’s dressing, his skin went really red and rashy underneath over the whole area. She was very quick to put the new dressing on and cover it up, but Christian spotted the redness and questioned her about it — otherwise she wasn’t going to mention it. All of a sudden she just said, “Oh, I did notice that, but just assumed it was a local skin reaction.” To make it worse, the first dressing she put on had been done so quickly it started peeling straight off, so Christian had to ask her to redo it.
The thing is, if he hadn’t noticed at the time, we could have lifted Chester’s t-shirt later in the day, seen his wiggly area all red and rashy, and gone into full panic mode thinking something serious was wrong and rushed him into hospital. Luckily, the redness went down and disappeared, so it must have just been a reaction to either the sticker coming off or the wipe she used — but either way, it’s never happened before.
We also got a copy of Chester’s blood and lab results for the last couple of months. Chester’s on the EsPhALL 2017 / COG-1631 trial (he’s on the COG side), so they’re supposed to keep a close eye on things like his liver numbers. We noticed on his results that his ALT levels have been all over the place — and quite high. They actually spiked towards the end of his intensive treatment back in March, and because they went so high then, we had to hold his chemo for two weeks. Apparently, the protocol has an upper limit for these numbers — if they’re higher, you’re meant to pause chemo until it drops back down, or do something about it. Imatinib, which Chester takes every day, is known for causing liver toxicity too.
Looking through his most recent results, the ALT levels have exclamation marks next to them nearly every week. We’re guessing that’s because they’re way higher than what’s normal for a child his age — probably because of all the meds — but no one has ever mentioned it to us, and we were honestly shocked when we saw the exclamation marks all the way down the list. Some weeks it’s in the 60s or 70s, but other weeks it’s shot up to 135, 217, even 261! The numbers go up and down, but there have been several weeks where it’s well into the 100s and 200s. According to the protocol, if ALT goes over five times the upper limit (which is usually about 40, so anything over 200), chemo should be paused until it drops back down, or something should be done about it — especially with imatinib, which is known for causing liver issues.
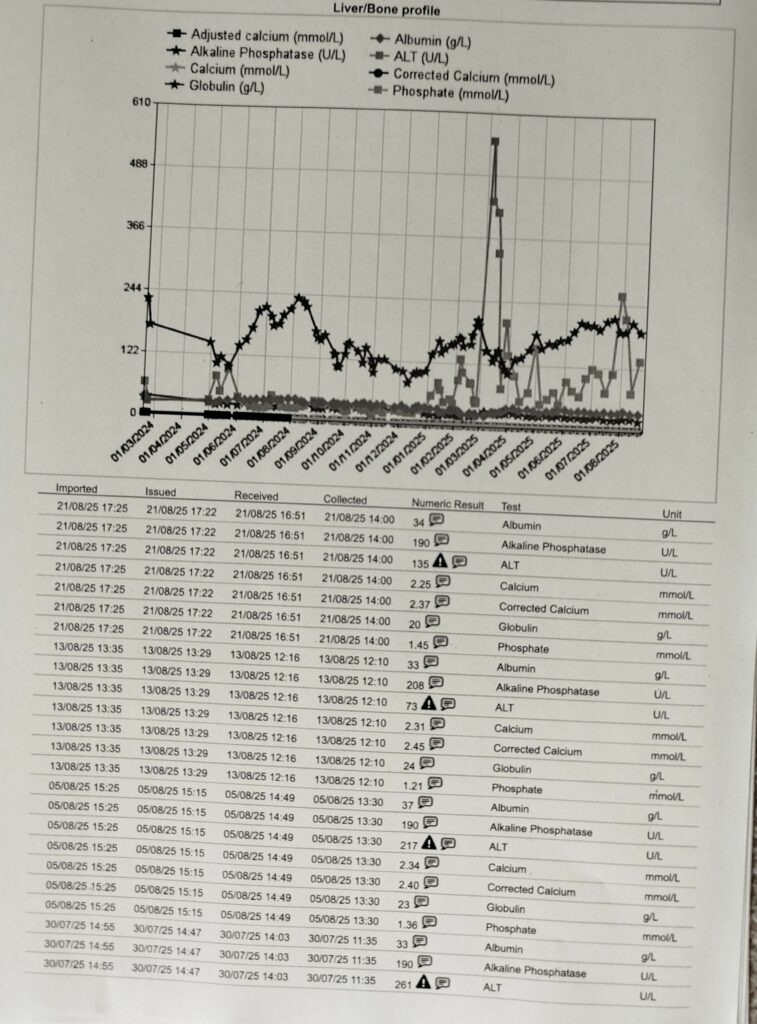
Looking back at the records, we actually saw that on the weeks when Chester’s ALT was over 200, his chemo doses were dropped to 50%. But nobody ever explained this to us at the time — we just assumed it was because his neutrophils were low (they’d dropped to 0.6 and 0.9 on those weeks). We were told “his liver is fine,” but we had to figure out ourselves that the dose reduction may also be due to his liver numbers, not just his neutrophils. Honestly, the communication just isn’t there.
Surely we shouldn’t have to work all this out ourselves. We’re supposed to be kept informed about changes in treatment — it’s our child and his safety. We’re just left guessing, and that’s not good enough.
And while we’re on the subject of blood results and communication, the delays are honestly ridiculous. For example, on the 5th of August the nurse came out to take Chester’s bloods at 1pm. We didn’t get a text with his results until the next day (6th August) at 12:14pm, but even then it just said she was waiting on Southampton to confirm his doses for the week. She couldn’t ask the local consultants at our hospital because they were both off — and, as usual, they always seem to be off at the same time, which really isn’t great.
At 5pm I chased up because we still hadn’t heard what doses to give (since we’d been on 50% doses the previous week for low neutrophils). The reply I got was basically, “I haven’t heard back from the main hospital, you’ll have to call them and find out yourself. If you don’t get an answer, I’ll chase up again tomorrow morning.” Not even that evening — the next morning! So I had to ring the CNS and get the answer myself.
But the thing is, if we’re waiting on a decision for the week’s doses, surely it should be a priority to chase up that day, not just leave it for the next morning — especially when Chester is on 50% doses and we need to know what to give that night. What’s the point in telling us to drop to 50% or go on a week’s hold if we end up giving the wrong doses for the first couple of days just because it takes them so long to communicate with us? It all just seems a bit pointless.
To make things even more fun, we asked for a top-up of ondansetron for this week — usually we get around 12 bottles at a time to keep us going so we’re not constantly worrying about running out. But this time, she could only give us 4 bottles, because (yet again!) both oncology consultants at the local hospital were off, and the pharmacy isn’t allowed to give us that amount in one go without their permission.
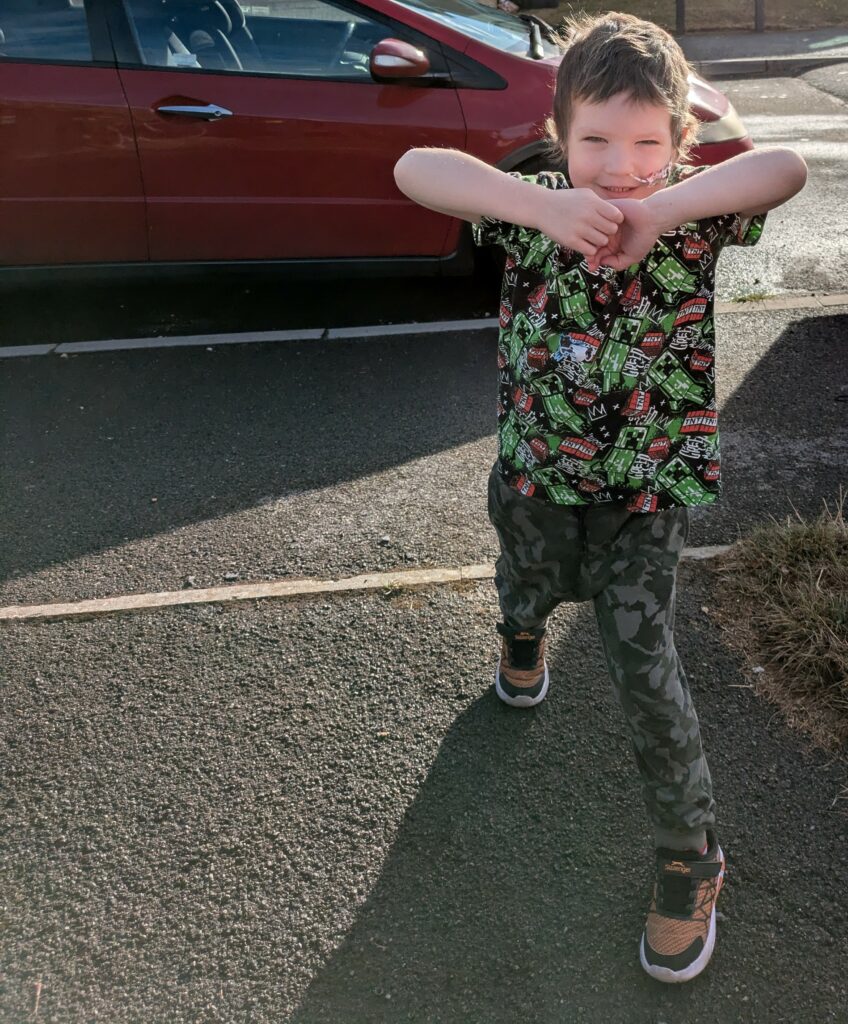
Even after everything we’ve been through, we’re still moving forward and keeping hope. We can finally see the finish line coming in April — and we can’t wait for Chester to be done with treatment, have his tubes out, and get back to just being a happy, normal little boy. The thought of all of us being able to move on and enjoy the simple things again is what keeps us going